Treatment option: Wim Hof Method
How the WHM could help post-concussion recovery by improving neurovascular coupling, among other things

If you haven’t heard of the Wim Hof Method by now, I can only assume you’ve been living under a rock. There’s so much information out there, including the instructional videos in the Wim Hof app (which I use every day), I’m not going to waste any time by going over the basics of the breathing method here.
Instead, I’ll focus on the specific ways this method can help with post-concussion recovery.
In discussions (and studies) about how the Wim Hof Method benefits the neuro-typical person, there’s a lot of emphasis on the benefits of creating blood cells that deliver more oxygen to the brain, and how the WHM (Wim Hof Method) delivers oxygenated blood supply to the deeper parts of the brain. The effects on the autonomic nervous system are also documented.
While these benefits are available to the person recovering from a concussion, I think the WHM helps on another level—and I would love to see this validated by a study. I believe the WMH helps an injured brain re-regulate neurovascular coupling, among other things.
What is neurovascular coupling and decoupling?
One of the primary ways that a brain becomes dysregulated after a concussion is with the decoupling of one’s neurological and vascular systems.
Here’s a definition of neurovascular coupling from Scholarpedia:
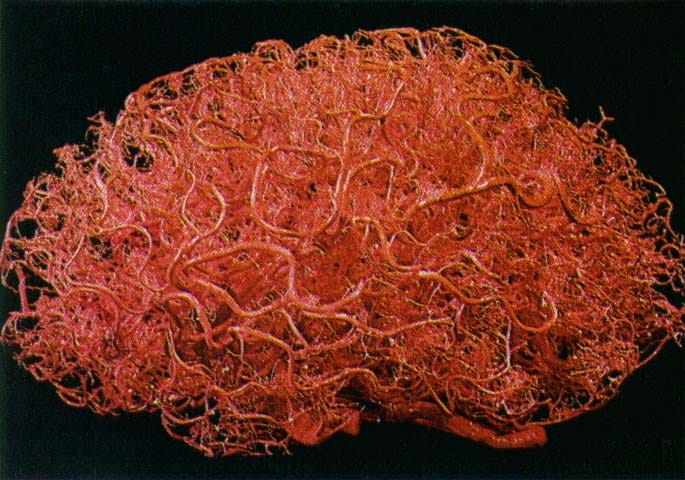
Neurovascular coupling refers to the relationship between local neural activity and subsequent changes in cerebral blood flow. The magnitude and spatial location of blood flow changes are tightly linked to changes in neural activity through a complex sequence of coordinated events involving neurons, glia, and vascular cells.
When this “complex sequence of coordinated events” gets disrupted by a head injury, parts of the brain that require blood flow for specific cognitive tasks will struggle to receive that blood flow.
So the neurons may be firing away, but the process that couples that firing with the delivery of blood flow is disrupted. (This may be due to damage of the vasculature, the nexus of blood vessels and neurons, disruption of the signaling process between neurotransmitters and the vascular system, a weakening of the signal between the brain and heart, or some combination of these things. The cause may also depend on which region of the brain is injured.)
Long term, the lack of regulated blood flow to areas of the brain causes further damage. In one study, neurovascular decoupling was associated with the severity of cerebral amyloid angiopathy, a neurodegenerative condition found in the brains of Alzheimer’s patients and retired NFL players alike.
Interestingly, neurovascular decoupling was also found to be a factor in the cognitive decline of people with type 2 diabetes. To me, this further supports the latest thinking that Alzheimer’s is a form of diabetes.
How might the Wim Hof Method help with neurovascular coupling?
So if we need to move from unhealthy decoupling back to healthy coupling, the question is: How do we go about doing that?
I suspect the WHM can help, in part because it is under our conscious control, and therefore helps create a “push-pull” between the neurological and vascular systems.
Out of curiosity, I once wore a neurofeedback device while doing WHM so I could record my brainwave patterns (using an app called Mind Monitor) during the breathing exercise. I was surprised to see an overall elevation of gamma waves, which are typically elevated during challenging cognitive tasks when multiple parts of the brain are working in concert.
My guess is that the top-down suppression of the urge to breathe during the breath-holding phase helps boost gamma. This cortical activity would also bring blood to the brain, perhaps strengthening neurovascular coupling.
There’s another way in which the WHM might help. If you do the standard breathing exercise in the WHM app and hear Wim’s voice guiding that breathing, you’ll hear him say, “It descends—the blood flow descends into the deeper parts of the brain.”
I presume Wim is referring to the university studies that looked at what happens with blood flow in the brain while doing Wim Hof breathing. And while “the blood flow descends into the deeper parts of the brain” may be a bit cryptic, my assumption is that the breathing exercise helps with perfusion in subcortical areas of the brain, which might help heal a damaged thalamus.
The Wim Hof Method does more than deliver oxygen to the brain
Although supplying the brain with oxygen is an important part of the WHM, it isn’t solely the oxygen that’s helping. After all, there are many ways to deliver oxygen to the brain, including hyperbaric oxygen chambers.
You can visit private clinics that offer hyperbaric oxygen as a treatment for people with brain injuries. While that treatment might offer symptom alleviation, I’m guessing the effects are temporary because you aren’t retraining or reacquiring the “complex sequence of coordinated events” in a neurologically active “push-pull” way that delivers blood flow to neurons.
To do that, you need to actively do things (the WHM, physical exercise, cognitive exercise, HRV training, etc) to reacquire and re-regulate these functions—from an internal locus of control rather than an external one.
The benefits of cold exposure for brain injury recovery
As with the breathing, the benefits of cold exposure for the neuro-typical person are fairly well established.
Those benefits include giving your cardiovascular system a workout, practicing top-down cognitive control over autonomic responses to external stressors, and releasing hormones that are beneficial to wellbeing.
It’s easy to see how those benefits would be especially helpful to someone recovering from a brain injury. But, as with the breathing, I think cold exposure is helping someone with a brain injury on another level.
Cold exposure helps re-establish the regulation of the autonomic nervous system and the proper balance between alertness and calm, which is something a person with a brain injury really struggles with—a condition known as dysautonomia (interestingly, one of the tests for identifying the scope of one’s dysautonomia involves breathing until you hyperventilate).
Cold exposure as nervous system and brain training
While listening to a recent episode of the Huberman Lab, I learned about something that brought the benefits of cold exposure into sharp focus for me.
As it turns out, the adrenaline produced by your body (by the adrenal glands) cannot cross the blood-brain barrier. The brain must produce its own adrenaline (which is called epinephrine, but it’s the same thing).
This means we can train our minds to remain calm—to not release adrenaline or to release controlled amounts—even as our body produces large quantities of adrenaline in response to stressors (such as the cold).
Now, when I take a cold shower in the morning, I visualize facing sudden and startling stressors. I feel the cold as a proxy for them. And I experience calm alertness—even a sense of play amidst the stress—as a state of mind that prepares me to face the inevitable stress of my day with equanimity.
Wim Hof Method points of emphasis for post-concussion recovery
Here are a few nuances that, for me, are points of emphasis in my ongoing practice of the Wim Hof Method, and may be helpful for you in your post-concussion recovery.
These points of emphasis are: timing the exercises to work with the circadian rhythm (the up and down-regulating cycles); using the pressure of the recovery breath; leaning on the mood regulation breathing technique to recover from neurological overstimulation, and using cold exposure to aid neuroplasticity.
Synchronizing the WHM with the circadian cycle
Since we’re a diurnal species, our waking hours begin with the “up-regulating” cycle— where we activate our nervous system and engage in periods of focus on exertion.
By starting your day with a breathing session and a cold shower (along with other behaviors like walking and light exposure), you give your nervous system strong signals that help move you toward alertness. You might do the breathing using the Fast setting in the app.
During this time period, other forms of WHM, including the Power breathing, can also help elevate your nervous system and your mind-body connection.
As afternoon turns to evening (around 5 or 6 PM) you can shift to using the breathing as a tool for calming. You might do the breathing using the Slow setting on the app, followed by the Mood Regulation breathing.
Use the pressure of the recovery breath
Wim Hof tells his students to do the 15-second recovery breath with their chin tucked down while bringing pressure from their body to the center of their head. You contract muscles in your body to bring this pressure to the head. As Wim puts it, the feeling is similar to what you might experience when you’re trying to take a difficult crap.
After a concussion, the brain and body may struggle with regulating blood pressure or dealing with spikes in blood pressure, which is one of the things that can make it difficult to exercise, especially if that exercise deals with rapid positional changes.
I believe that by placing an emphasis on pressurizing the recovery breath, we can help retrain ourselves to deal with and regulate this kind of pressure.
Turn down the fight or flight response with Mood Regulation breathing
A hallmark of post-concussion syndrome is an elevated (overactive) fight or flight response. Stressors (including simple things like loud noises or sensory-rich environments) can easily push you into extreme levels of agitation.
Breathing is like an access panel to the nervous system. There are many forms of breathing that can calm the nervous system. By merely exhaling for a longer time than you’re inhaling, you can reset yourself. For example, exhaling for a count of 6, inhaling for a count of 4.
But for my money, nothing is as effective and swift as the WHM Mood Regulation breathing. It takes about 10 to 15 minutes and by the time you’re done, the feeling of reset can be so profound, it’s almost akin to waking up to a new day after a terrible one.
Time cold exposure to aid neuroplasticity
Since cold exposure is something that can help trigger neuroplasticity, you can time a cold shower or bath with other treatments that spur neuroplasticity. For example, if you have a set of physical or occupational therapies that trigger your symptoms, you might follow that with a cold shower.
For more information about the steps involved with neuroplastic change, see these segments of the Huberman Lab:
Wrapping up
The Wim Hof Method has many benefits for people without brain injuries, but it can be a vital tool for people recovering from one. The breathing and cold exposure have separate but synergistic benefits that can be further enhanced by paying attention to specific points of emphasis.
My guess is that the Wim Hof Method may offer us a way to steadily reestablish and strengthen neurovascular coupling, especially when part of a physical and cognitive exercise routine. It may also help support the process of neuroplastic change.
Last, but certainly not least, it gives someone suffering from nervous system overload a very practical tool for reseting so they can capably answer the questions that life is asking of them.
Brainwave is an informational resource for people whose symptoms haven’t resolved after a concussion or mTBI. I endeavor to present this information in a clear and concise way, spelling out what’s backed by science and what remains unknown. Nothing here is meant as a substitute for professional medical advice, diagnosis, or treatment. I am not a physician or a healthcare practitioner of any kind; I’ve simply had a lot of sports-related concussions and had to learn this stuff the hard way. If you found this information helpful or know someone who might benefit from it, please share and subscribe to Brainwave.



